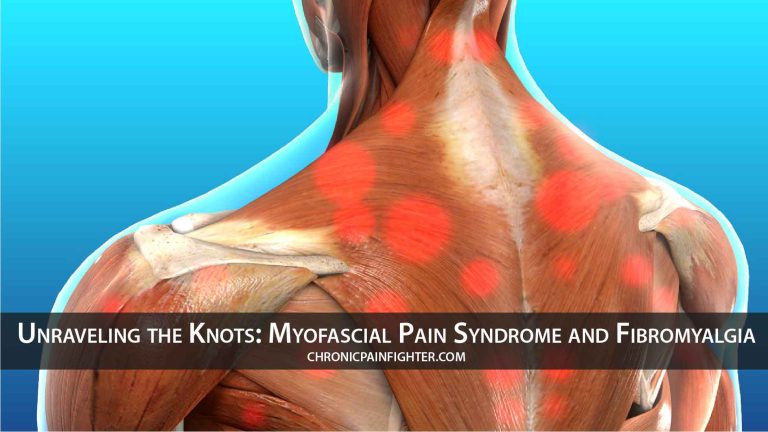
Chronic pain is a debilitating experience, and when it affects muscles and soft tissues, it can significantly impact daily life. Two conditions often intertwined and sometimes confused are myofascial pain syndrome (MPS) and fibromyalgia. While distinct, they share similarities in symptoms and can coexist, making diagnosis and treatment challenging. This article delves into the complexities of these conditions, exploring their causes, symptoms, and management strategies.
Understanding Myofascial Pain Syndrome
Myofascial pain syndrome (MPS) is a chronic pain condition characterized by the development of trigger points – hypersensitive areas within taut bands of muscle. These trigger points can refer pain to other parts of the body, creating a complex pain pattern that can be difficult to pinpoint.
Causes of MPS:
- Muscle overuse or strain: Repetitive motions, poor posture, and strenuous activities can lead to muscle tension and trigger point formation.
- Trauma: Injuries, such as whiplash or falls, can trigger MPS.
- Stress and anxiety: Psychological stress can contribute to muscle tension and trigger point development.
- Underlying medical conditions: Conditions like arthritis, diabetes, and thyroid disorders can sometimes trigger MPS.
Symptoms of MPS:
- Localized pain: Pain is often concentrated in specific areas, such as the neck, shoulders, back, hips, or legs.
- Trigger points: Tender spots within muscles that cause pain when pressed.
- Referred pain: Pain radiating from the trigger point to other areas of the body.
- Muscle stiffness and tightness: Limited range of motion and difficulty moving the affected muscles.
- Headaches: Trigger points in the neck and shoulders can often cause headaches.
Fibromyalgia: A Widespread Pain Disorder
Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, and other symptoms that affect the entire body. Unlike MPS, which focuses on localized trigger points, fibromyalgia involves a more generalized pain experience.
Causes of Fibromyalgia:
- Genetics: A family history of fibromyalgia increases the risk of developing the condition.
- Trauma: Physical or emotional trauma can trigger fibromyalgia.
- Infections: Some viral or bacterial infections have been linked to fibromyalgia.
- Autoimmune disorders: Fibromyalgia may coexist with autoimmune disorders, such as rheumatoid arthritis.
Symptoms of Fibromyalgia:
- Widespread pain: Pain is felt in both sides of the body, above and below the waist, and affecting the axial skeleton (neck, back, and chest).
- Fatigue: Persistent and debilitating fatigue that can interfere with daily activities.
- Sleep disturbances: Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep.
- Cognitive difficulties: Brain fog, memory problems, and difficulty concentrating.
- Mood disorders: Anxiety, depression, and irritability are common in fibromyalgia.
- Other symptoms: Headaches, irritable bowel syndrome, and sensitivity to light, sound, and touch.
The Overlap Between MPS and Fibromyalgia
The lines between MPS and fibromyalgia can blur, as they share several common symptoms. Both conditions involve muscle pain and tenderness, and trigger points can be present in both. Furthermore, MPS can sometimes be a contributing factor to fibromyalgia, as trigger points can contribute to widespread pain and fatigue.
Key Differences:
- Pain distribution: MPS pain is typically localized to specific areas, while fibromyalgia pain is widespread.
- Trigger points: Trigger points are a hallmark of MPS, but they are not always present in fibromyalgia.
- Other symptoms: Fibromyalgia is associated with a wider range of symptoms, including fatigue, sleep disturbances, and cognitive difficulties.
Diagnosis and Treatment
Diagnosing MPS and fibromyalgia can be challenging, as there are no definitive tests. Diagnosis relies heavily on a thorough medical history, physical examination, and ruling out other conditions.
Diagnosis:
- Medical history: A detailed account of symptoms, including their onset, duration, and location.
- Physical examination: Palpation of muscles to identify trigger points and assess tenderness.
- Imaging studies: X-rays, MRIs, and ultrasounds may be used to rule out other conditions.
- Blood tests: To rule out other conditions, such as infections or autoimmune disorders.
Treatment:
- Pain management: Over-the-counter pain relievers, prescription medications, and physical therapy can help manage pain.
- Trigger point therapy: Techniques like massage, stretching, and dry needling can help release trigger points.
- Lifestyle modifications: Regular exercise, stress management, and good sleep hygiene can improve symptoms.
- Cognitive behavioral therapy (CBT): CBT can help individuals develop coping strategies for managing pain and improving quality of life.
Living with MPS and Fibromyalgia
Living with MPS and fibromyalgia can be challenging, but with proper management, individuals can lead fulfilling lives. It’s important to work closely with a healthcare professional to develop a personalized treatment plan that addresses individual needs.
Tips for Managing MPS and Fibromyalgia:
- Stay active: Regular exercise, even gentle activities like walking or swimming, can help improve muscle function and reduce pain.
- Manage stress: Stress can exacerbate symptoms. Practice relaxation techniques like yoga, meditation, or deep breathing.
- Get enough sleep: Aim for 7-8 hours of quality sleep each night.
- Eat a healthy diet: A balanced diet can provide essential nutrients and support overall health.
- Join a support group: Connecting with others who understand your condition can provide emotional support and practical advice.
Conclusion
Myofascial pain syndrome and fibromyalgia are complex conditions that can significantly impact quality of life. While they share similarities, understanding their distinct characteristics is crucial for accurate diagnosis and effective treatment. By working closely with healthcare professionals and adopting a holistic approach to management, individuals can find relief from pain and improve their overall well-being.