Fibromyalgia, a chronic condition characterized by widespread musculoskeletal pain, fatigue, and other symptoms, often goes hand-in-hand with digestive problems. This connection, known as the gut-brain axis, highlights the intricate relationship between the digestive system and the central nervous system.
The Gut-Brain Axis: A Complex Connection
The gut-brain axis is a two-way communication system. Your gut, home to trillions of bacteria, sends signals to your brain, influencing mood, sleep, and even pain perception. Conversely, your brain can influence gut function, affecting digestion, nutrient absorption, and even the composition of your gut microbiome.
Fibromyalgia and Bowel Issues: A Common Link
Many people with fibromyalgia experience a range of bowel issues, including:
- Irritable Bowel Syndrome (IBS): IBS is a common disorder characterized by abdominal pain, bloating, gas, diarrhea, and constipation. It’s often associated with fibromyalgia, and the two conditions may share similar underlying mechanisms.
- Constipation: Many people with fibromyalgia experience constipation, which can be caused by pain medication, lack of physical activity, and changes in gut motility.
- Diarrhea: Diarrhea can also occur in fibromyalgia, often related to IBS or other digestive disorders.
- Bloating and Gas: These symptoms are common in both fibromyalgia and IBS, and they can be caused by changes in gut motility and bacterial imbalances.
- Gastrointestinal Pain: Abdominal pain is a frequent complaint in fibromyalgia, and it can be difficult to distinguish from pain related to bowel issues.
Why Are Bowel Issues Common in Fibromyalgia?
The exact reasons why bowel issues are so common in fibromyalgia are still being investigated, but several factors are likely involved:
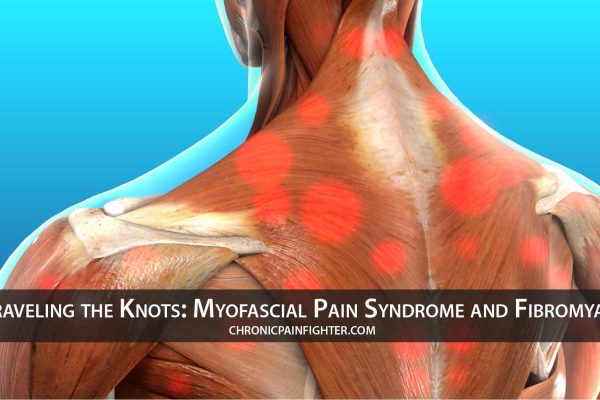
- Central Sensitization: Fibromyalgia is characterized by central sensitization, a condition where the brain becomes hypersensitive to pain signals. This hypersensitivity can extend to the gut, leading to increased pain perception and altered gut motility.
- Neurotransmitter Imbalances: Neurotransmitters like serotonin and dopamine play a role in both gut function and pain perception. Imbalances in these neurotransmitters may contribute to both fibromyalgia and bowel issues.
- Gut Microbiome Dysbiosis: The gut microbiome, the community of bacteria living in your gut, plays a crucial role in digestion, immunity, and even brain function. Dysbiosis, an imbalance in the gut microbiome, has been linked to both fibromyalgia and bowel issues.
- Inflammation: Chronic inflammation is a hallmark of fibromyalgia, and it can affect the gut, leading to increased permeability and inflammation in the digestive tract.
Managing Bowel Issues in Fibromyalgia
Managing bowel issues in fibromyalgia requires a multi-faceted approach that addresses both the physical and psychological aspects of these conditions. Here are some strategies:
- Dietary Changes: A balanced diet rich in fiber, fruits, and vegetables can help regulate bowel function and reduce inflammation. Consider working with a registered dietitian to develop a personalized meal plan.
- Stress Management: Stress can exacerbate both fibromyalgia and bowel issues. Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises.
- Regular Exercise: Regular physical activity can improve gut motility and reduce constipation. Start with gentle exercises and gradually increase intensity as tolerated.
- Medication: Over-the-counter medications like fiber supplements and laxatives can help manage constipation. For IBS, your doctor may prescribe medications to relieve pain, reduce bloating, or regulate bowel movements.
- Probiotics: Probiotics are live bacteria that can help restore balance to the gut microbiome. Consider taking a probiotic supplement or consuming probiotic-rich foods like yogurt and sauerkraut.
- Prebiotics: Prebiotics are types of fiber that feed the beneficial bacteria in your gut. Include prebiotic-rich foods like bananas, onions, and garlic in your diet.
- Lifestyle Modifications: Avoid trigger foods that worsen your symptoms, stay hydrated, and get enough sleep.
The Importance of Collaboration
It’s crucial to work closely with your doctor and other healthcare professionals to manage both fibromyalgia and bowel issues. They can help you identify the underlying causes of your symptoms, develop a personalized treatment plan, and monitor your progress.
Conclusion
The connection between fibromyalgia and bowel issues is complex and multifaceted. Understanding the gut-brain axis and the factors that contribute to these conditions is essential for effective management. By adopting a holistic approach that addresses both physical and psychological factors, you can improve your digestive health and overall well-being. Remember, you are not alone in this journey, and with the right support, you can navigate these challenges and live a fulfilling life.